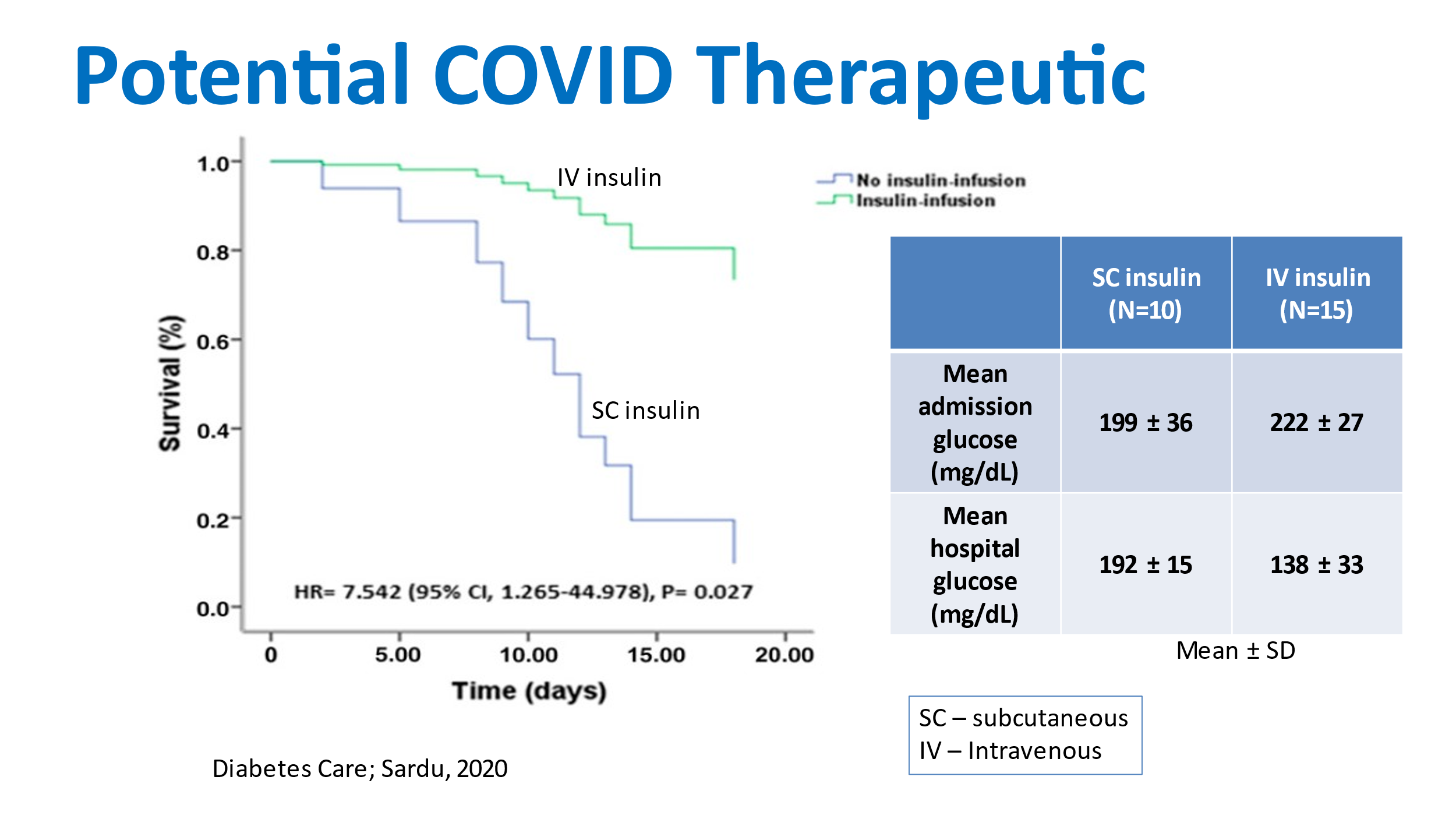
 Lowering glucose levels with IV insulin significantly lowers COVID mortality rate.
An Italian study by Sardu demonstrated that when the blood glucose level was lowered through use of IV insulin, from the time of admission, COVID mortality rates were significantly decreased. In this non-randomized study, patients admitted to the hospital with COVID were offered the choice of lowering their glucose levels with subcutaneous (SC) insulin injections or IV insulin. The patients who chose SC insulin had average hospital glucose levels of 192 mg/dL, versus 138 mg/dL in the patients treated with IV insulin. The patients treated with IV insulin had significant lowering of their cytokine response, abnormalities on chest CT, and mortality rates.
For more information check out this article in Diabetes Care titled Outcomes-in-Patients-With-Hyperglycemia-Affected by COVID-19: Can We Do More on Glycemic Control?
Elevated glucose at admission and during hospitalization predicts increased mortality rates in COVID
A U.S. study by Bode on 570 COVID patients demonstrated that the group of patients (n= 184) with either diabetes or uncontrolled hyperglycemia (> 180 mg/dL) had a mortality rate of 28.8%, versus a mortality rate of 6.2% in the group of patients (n= 386) without diabetes or uncontrolled hyperglycemia. The average hospital glucose level of the diabetes/uncontrolled hyperglycemia group was 179 mg/dL, versus 117 mg/dL in the group without diabetes/uncontrolled hyperglycemia. This study can be found in the Journal of Diabetes Science and Technology, titled Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States Average glucose value, lowest glucose value, and glucose variability all predict mortality rates in ICU patients with and without diabetes A U.S. study of 52,107 ICU patients demonstrated that time-weighted average glucose values were associated with hospital mortality rates, as seen below. This association was true for both diabetic and non-diabetic patients. From the graph, it can be seen that the average glucose value should be kept below 125 mg/dL for both diabetic and non-diabetic patients. In the FUSION systems first in human clinical study, with a glucose control range of 100-140 mg/dL, the participants average glucose value was 123 mg/dL. 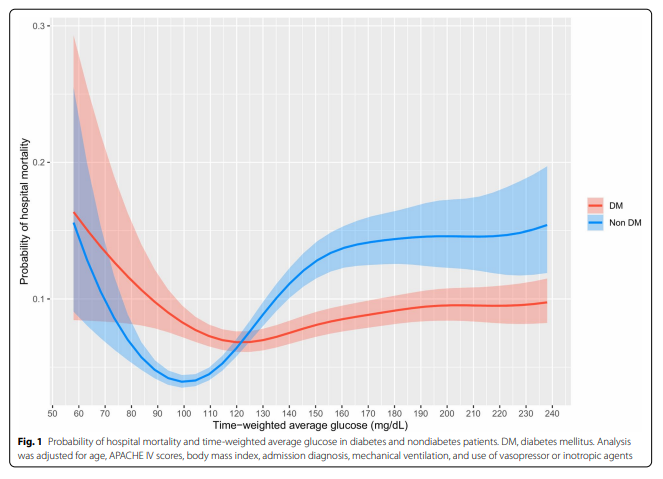 Fong, BMC Anesthesiology, 2022
This same study demonstrated the association between minimal glucose values experienced by ICU patients and mortality rates, as seen below. From the graph, it can be seen that hypoglycemic glucose values (< 70 mg/dL) should be avoided in ICU patients at all costs. In the FUSION systems first in human clinical study, none of the study participants experienced glucose values less than 70 mg/dL.
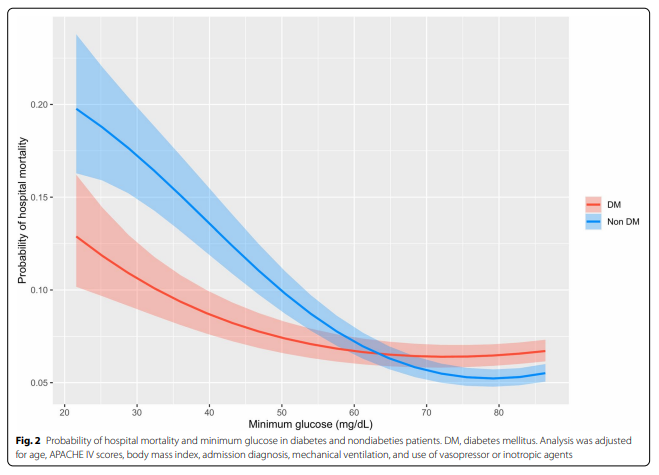 Fong, BMC Anesthesiology, 2022
Finally, this same study demonstrated the importance of minimizing glucose variability. This study used glucose coefficient of variation as a measure of variability, and as can be seen from the graph it is important to maintain the coefficient of variation less than 25% for both diabetic and non-diabetic patients. In the FUSION systems first in human clinical study, the participants average coefficient of variation was 20%.
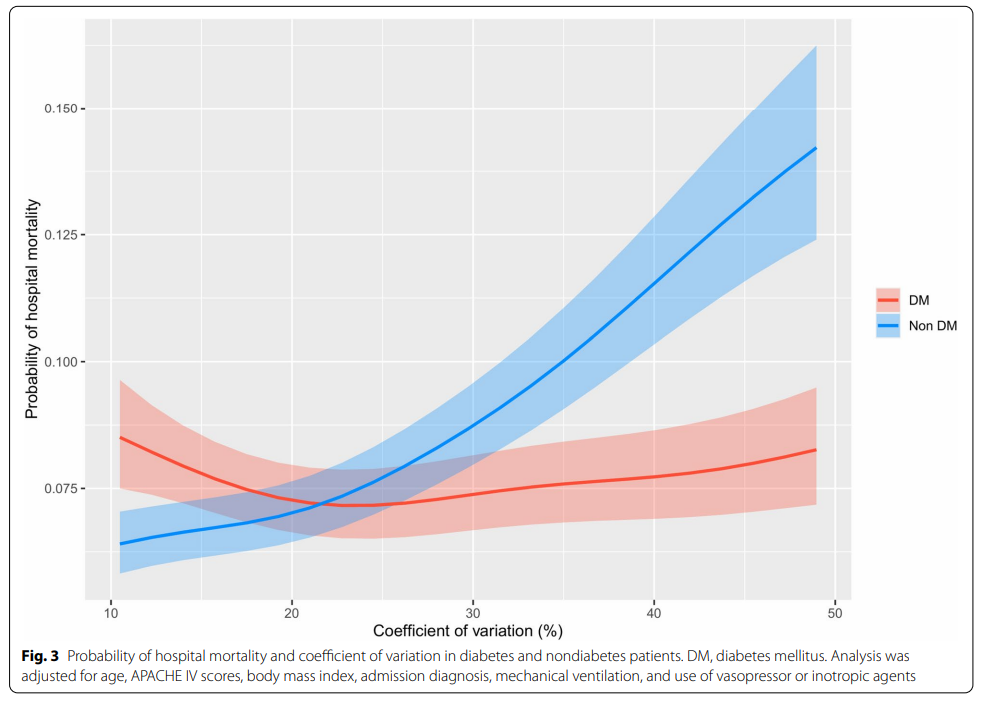 Fong, BMC Anesthesiology, 2022 This large U.S. study can be found in BMC Anesthesiology under the title Glycemic control in critically ill patients with or without diabetes. Or you can go to the clinicaltrials.gov website to view the FUSION systems first in human study |